Health Systems Awareness, Resilience, and Transformation
Equipping healthcare policymakers with the capabilities to transform healthcare systems
The challenge:
Medicine is only effective if patients can access it. The pandemic highlighted some of the huge challenges that health systems, major public health agencies and healthcare leaders face. Systemic problems such as decreasing levels of public and political trust, funding, and workforce challenges, threaten patient care and access to medicines.
Changing demographics, greater demand, rapidly evolving technology, and information overflow pose additional challenges to systems, patients, and healthcare workers.
A Sub-Saharan Africa Value and Access team at a global medicines company had the vision to create a Health Economics and Outcomes Research (HEOR) course for key policymakers and leaders to strengthen health systems and build relationships. However, it was missing the component of moving from ‘knowing to doing’ and they wanted to add a module that would prepare learners to put what they learned into practice.
We were asked to design a program for 45 healthcare policymakers across 9 countries, to help them enact change, to be delivered in tandem with HEOR training provided by the Vienna School of Clinical Research.
The spark:
We wanted to enable changemakers to be more adaptive in their leadership of change and flexible in the face of an ever-changing landscape.
Our research and experience told us that healthcare transformation is not only technical but deeply cultural. Across systems, entrenched habits, resistance to change, and siloed thinking prevent effective adoption of new models such as value-based care, strategic purchasing, or digital health solutions.
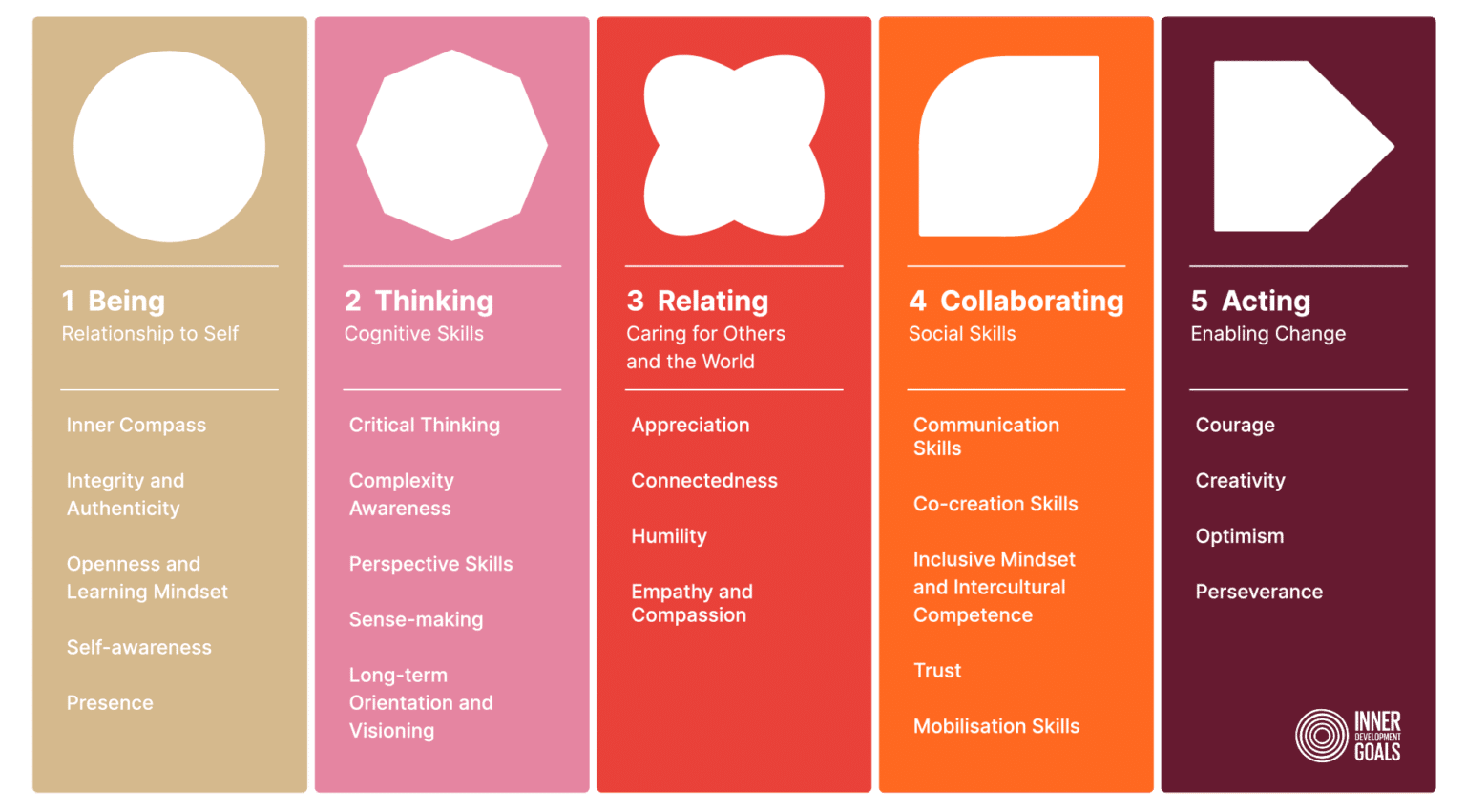
Building a culture of change involves structured stakeholder engagement, shared vision creation, and capacity-building in adaptive skills like systems thinking, collaborative learning, and accountability. Healthcare workers, policymakers, and community actors alike need support to question old norms, embrace experimentation, and co-create new practices that prioritise equity, quality, and efficiency.
The proposal:
We created a four-part virtual pilot program underpinned by systems sensemaking activities and feedback loops, comprising scientifically validated tools and methods to build capability, increase self, interpersonal and systemic awareness, and provide safe environments to build strategies and practice communicating transformation plans and giving feedback.
The program was run over four sessions with systems sensemaking activities such as narrative action research, woven into the design.
Session 1: Introduction to systems awareness
Basics of systems thinking and transformation
Session 2: Self-awareness via Immunity to Change
Exploring barriers to change
Session 3: Building your systems strategy mandala
Building a strategy for changemaking and mobilisation considering the entire system
Session 4: Communicating your systems strategy mandala
Practice collaboration, communication and feedback
Results:
For the medicines company:
As part of the Health Systems Awareness, Resilience and Transformation pilot module we collected data in several formats:
Narrative Action Research - an intervention that was sent out by learners into their systems and was answered by both health care professionals and patients
Systems Strategy Mandalas - created by our learners in the practical part of the module
In session polls and quizzes
The combined use of both the systems mandalas and narrative research has provided us with a unique insight into Sub-Saharan Africa. From this we were able to summarise key emerging themes around access.
The data provided powerful, ground-level insights into the real-world barriers, behaviors, and adaptive capacities shaping healthcare systems across the region.
This work helps us to tackle access issues by revealing the underlying systemic patterns such as bottlenecks in financing, workforce gaps, fragmentation, and cultural barriers that medicines alone cannot solve. By understanding how health systems behave in real-life contexts, the organization can co-create targeted, high-impact interventions that align with local realities, strengthen trust, and support long-term, sustainable access.
For learners
Changemakers told us that their knowledge had improved significantly, and they would like to continue learning, spending more time on practical tools and systems resilience.
Facilitators were given a 5 star rating by learners
Comments included:
“The building of the mandala was the icing in the cake. It was a great tool to systems thinking, issues identification, priority setting and improvement planning”
“The creation and analysis of the mandalas was a "Eureka" moment for me. I now see how a group can tackle a problem in a non-confrontational manner to reach joint solutions.”
There are future plans for follow-up training where we will measure the behavioural change of these sessions.
We asked changemakers how they would integrate practices and tools into their health systems? They said….
“ combination of the technical challenges and adaptive challenges cause conflict between various stakeholders in the industry. Adaption of changes will first have to happen before the technical issues can be sorted out. ...”
“With our health system still under development, A mandala will be quite useful in identifying the issue at hand and how it easily set the flow of solving the issue.”
“The changes are necessary to improve the systems. I would focus on developing the Mandala into an implementation project...”
“...continuous engagement across all major stakeholders in the value-chain to throw more light on the key deliverables and how the outcomes can help improve the system. Data gathering and evaluation are the needed skills needed to overcome the current challenges confronting the system.”